Reflection: realities and risks
Post date: 09/05/2017 | Time to read article: 3 minsThe information within this article was correct at the time of publishing. Last updated 14/11/2018
The importance of lifelong learning in medicine is well-recognised. Dr Vanessa Perrott, Head of Education and Delivery, and Dr Karen Ellison, Medicolegal Adviser, discuss reflective practice as part of this process
Read this article to:
- Understand the importance of lifelong learning
- Discover the benefits and risks of reflection
- Complete our CPD-accredited e-learning module on Reflection
Reflective practice is an expected part of any medical professional’s life; the GMC is unequivocal on this.1 The pedagogy behind reflection is well-recognised and can be summed up by the following statement: “We do not learn from experience … we learn from reflecting on experience.”2
As an aspect of deep and lifelong learning, reflection needs to be built into our everyday practice – no matter where we are in our specialist journey. It may be formalised into specialist training programmes as part of a portfolio of learning and continued into appraisals, significant events and performance reviews; before the cycle begins again when seniors are asked to take on a supervisory role of those in specialist training.
Figure 1: The Action Research Model for lifelong learning3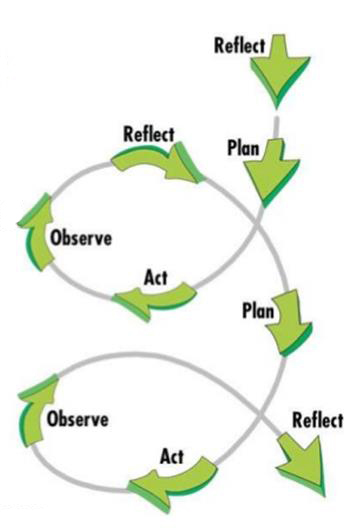
The ability to reflect on experiences is an important skill for all doctors. While it may be that we are practising optimally, it is likely that there are areas of our practice that could be improved. Reflection is an important part of maintaining competence and contributes to quality improvement. It helps provide a way of self-monitoring our performance so that we can both identify those areas where we are practising optimally, and also define learning needs and areas for improvement. Evidence of reflection may also be called for if a doctor has a complaint or claim against them.
What are the benefits of reflection?
- It enables you to gain greater insight into how you think and act (ie, develops your emotional intelligence).
- It helps you develop a new way to tackle problems and explore them in a structured and meaningful manner. This may reduce risks for the future, or provide a better way to tackle a similar problem next time.
- Using the skills of reflection in your everyday practice will help you reflect on incidents, good and bad, to make changes for safer practice.
- Reflective practice can help prevent burnout and increase job satisfaction by identifying and promoting the good parts of your job, whilst seeking to adapt those aspects that are less satisfying.
Harms of reflection
One of the biggest risks of reflection, in our view, is failure to reflect. “A doctor who appears to be failing to reflect properly could be criticised for lacking insight, making an employer or regulator consider them a risk to patients.”4
Learning without reflection is a waste. Reflection without learning is dangerous
Confucius
The products of reflection, for example, a written portfolio, need to be professional at all times. This means reflections need to be objectively written and demonstrate respect for patient confidentiality. While the GMC actively encourages learning from patients, where possible this information should be anonymised. The recent case of a trainee’s reflection in her portfolio being used as evidence against her highlighted the potential risks if these principles aren’t followed.5 If your reflections are requested as part of a case or investigation, and you are concerned that they may put you in a vulnerable position, contact one of our medicolegal advisers.
To maximise the benefits of reflection and minimise the harms, we suggest you:
- ensure conditions for reflection are appropriate
- ensure the process of reflection is clear
- ensure the products of reflection are appropriate.
Conditions for reflection6
- Time and space
- Good facilitator
- Curricular or institutional environment
- Emotionally supportive environment.
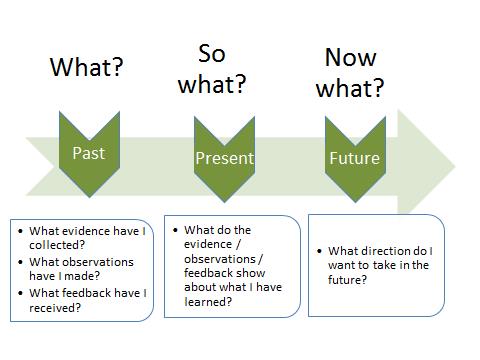
Process of reflection
Summary
Medical Protection knows that time is a precious resource for every doctor. Finding time-efficient ways to engage in the process of reflection and deliver useful and safe products from this, is crucial in developing the lifelong habit of reflection.
References
- http://www.gmc-uk.org/guidance/ethical_guidance/11817.asp
- Dewey J. 1938 cited in Beard C and Wilson J P. Experiential Learning: A Handbook for Education, Training and Coaching (Third Edition). London; Kogan Page; 2013.
- Kemmis, S and McTaggart R (eds). The Action Research Planner. Victoria, Australia: Deakin University Press; 1988.
- Davies M and Kramer D. Reflection: how to reduce the risks, BMJ Careers 2016.
- Matthews-King A. Trainee’s portfolio ‘used as evidence against them’ in legal case Pulse. 15 April 2016.
- Moon, J. Reflection in Learning and Professional Development Theory and Practice. London: Kogan Page; 1999.
Find out more
For further tips and a deeper understanding of reflection, you may want to complete our CPD-accredited e-learning module on reflection

