Learning from cases: Gastroenterology
Post date: 17/11/2023 | Time to read article: 8 minsThe information within this article was correct at the time of publishing. Last updated 06/12/2023
Read this resource to:
- Understand common themes from gastroenterology cases in the UK in which we have supported members.
- Receive tailored advice and key recommendations to help you reduce risks in the future.
Gastroenterology is a unique field, so the advice you receive needs to be equally specialised.
As a Medical Protection member, you benefit from more than 130 years of experience defending doctors and other healthcare professionals. That isn’t just a number – it’s more than 13 decades of specialist expertise that we use to protect you long into the future.
The team at Medical Protection, including medicolegal experts and cases and claims specialists, have delved into a huge range of gastroenterology cases to analyse the common reasons for claims and the different case types, to help keep you up to date with the current trends and provide insights into the gastroenterology claims and complaints landscape.
We hope you find this a useful source of guidance and advice, empowering you to protect yourself throughout your career.
Introduction
Gastroenterology has developed into a branch of medicine involving many different and advanced therapeutic endoscopic procedures. Each procedure has associated inherent risks and complications. Sometimes, endoscopy procedures do not go as planned, but the impact is inconsequential. However, a series of minor adverse events may culminate in a significant adverse event. Medicolegal cases are not uncommon due to the significant impact the complications can have on patients’ lifestyles.
We know that population-based bowel cancer screening exposes healthy, asymptomatic individuals to sedation and invasive procedures. Most cases reported to Medical Protection relate to elective procedures undertaken outside the NHS.
Claims in gastroenterology can sometimes lead to large financial settlements. The value of a settled claim will often include compensation for care and loss of earnings, if applicable, in addition to an award for the damage that resulted from a breach of duty. Complications can result in the patient requiring additional surgery – such as an ileostomy or colostomy – and, in some cases, death. The value of each claim varies enormously, with our highest gastroenterology total case payment (claimant damages, costs and legal costs) 2006-2015, being well in excess of £700,000.
We understand that you work in complex and pressured environments. We know following feedback from members that experiencing a medicolegal case can be concerning and a source of stress. At Medical Protection we want to share our knowledge, experience and expertise with you to provide professional support that we hope you find valuable.
Analysis
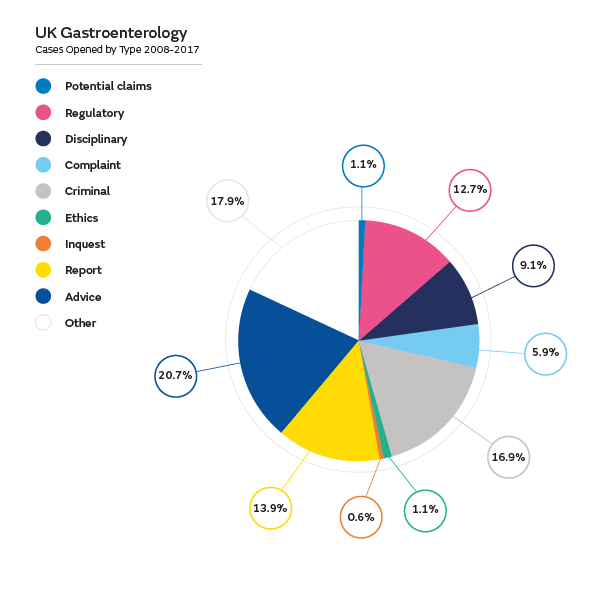
We’ve analysed the support Medical Protection has provided to UK-based gastroenterology members in over 300 cases between 2008 and 2017. We have provided advice and assistance in writing medical reports and supported our gastroenterology members in relation to claims (demands for monetary compensation that embodies allegations of negligence), potential claims (intimations from a claimant of a possible claim for compensation), complaints, GMC investigations, local disciplinary procedures, inquests and criminal investigations.
We have analysed all claims, including those defended, not pursued and settled. We feel that sharing our learnings from the reasons patients decide to take action is valuable, as well as the reasons why claims are settled.
Claims: Procedures and contributory factors
Delay in diagnosis or treatment
Almost half of the claims related to a delay in diagnosis or treatment, and of these claims the highest number of claims related to the delay in diagnosis or treatment of cancer of the gastrointestinal tract, including stomach, pancreas, small and large bowel. We acknowledge that some stomach and pancreatic cancers can be more difficult to diagnose in patients who present with vague symptoms. Patients often claimed for compensation if they felt their gastroenterologist should have detected their cancer earlier.
In some cases, there were allegations of delays in diagnosing Crohn’s disease, ulcerative colitis or gallstones. In our analysis of claims, we identified four key themes of contributory factors behind delays in diagnosis or treatment:
- misdiagnosis of benign disease
- mismanagement/communication of test results
- failure to follow current national guidelines
- inadequate safety netting advice resulting in delayed re-presentation.
Misdiagnosis of benign disease
There were claims of delays in diagnosis where patients had already been investigated for the same or similar symptoms and had previous negative test results. In some cases, initial investigations for patients with bowel symptoms were reported as benign, for example, liver lesions on a CT scan being reported as haemangiomas. Allegations were made that if a colonoscopy procedure had been done sooner, large bowel cancer with liver metastases would have been diagnosed sooner. There were a few cases where symptoms were attributed to helicobacter pylori, but the patients were later found to have stomach cancer. There were some cases where pancreatic lesions on a CT scan were reported as benign pancreatic cysts.
Mismanagement/communication of test results
Our analysis of claims highlighted that inadequate processes to follow up test results
can lead to claims alleging delays in diagnosing cancer. We have settled claims where inadequate communication of histopathology biopsy results between hospitals, gastroenterologists and patients had resulted in months of delays in commencing treatment. Contributing factors included one case where results had been filed in the patient’s records by administrative staff without being reviewed and actioned by a gastroenterologist. Another case saw delays in a patient receiving biopsy results from both their gastroenterologist and GP.
Failure to follow current national guidelines
The British Society of Gastroenterology (BSG) and NICE regularly update their guidelines relevant to the field of gastroenterology. We have had a few claims where the gastroenterologists had used out of date national guidelines that had been superseded. This resulted in failures to undertake annual surveillance colonoscopies, as suggested in the relevant guideline, resulting in delays in diagnosing of cancers.
Inadequate safety netting advice resulting in delayed re-presentation
In our analysis of claims of delays in cancer diagnosis, some joint allegations of negligence were made against GPs, NHS hospital trusts and gastroenterologists providing private healthcare. Diagnosing some cancers in patients who present with vague symptoms can be challenging. It is not uncommon for patients to consult healthcare professionals a few times before suspected cancer referrals are made. Some cancers are diagnosed following emergency admission to hospital. Patients were more likely to take action if they were uncertain why, when and with whom they should have re-consulted and if they had difficulty making a repeat appointment.
Our highest gastroenterology case total payment was in excess of £700,000.
Endoscopic complications
The second most frequent claim was complications following an endoscopic procedure.
In more than 10% of claims from our data the patient experienced a perforation, specifically during gastroscopy, colonoscopy, sigmoidoscopy, and endoscopic retrograde cholangiopancreatography (ERCP). The most frequent perforation occurred during a colonoscopy. The common contributing factors leading to claims being settled following perforation were:
- inadequate consent
- inadequate documentation
- delay in managing complications.
When the documentation around consent was reviewed it was judged to be inadequate by our experts in some claims following perforation during an endoscopy procedure. The detail of the risks on the consent forms that were used was considered lacking and there was no documentation in the patients’ records to confirm what had been discussed with the patients. In addition, the patient information leaflets given sometimes provided very limited information. Some patients developed pancreatitis following ERCP and made claims of negligence against their gastroenterologist. A number of these claims were settled because the consent process was considered to lack specific detail about the ERCP procedure and the risk of complications including pancreatitis. Claims were more likely to be defended when there was clear documentation of all the steps to provide evidence of a detailed interactive discussion with the patient.
A BSG working party has developed a standards framework that sets out the standards of performance and safety to improve the quality and availability of ERCP in the UK.
The BSG guidelines recommend: “It is particularly important that patients are aware of the risks of perforation and bleeding, that complications may be delayed and that surgical intervention may be required. The magnitude of risk should be clearly documented.”
In some claims it was alleged that perforations undetected at the time of the endoscopy should have been diagnosed and treated sooner. Expert witnesses have criticised some gastroenterologists for insufficient monitoring leading to delays in detecting deterioration in vital patient signs. Cases were more likely to be settled if the documentation was limited, in particular if more immediate action to manage complications was necessary.
Patient complaints: common themes
When we analysed the patient complaints reported to Medical Protection there were some similar themes to the claims, but also some new themes:
- The clinical judgment of the doctor or the management of the care of the patient was a reoccurring theme in nearly half of the complaints, for example not keeping the patient informed/lack of explanation of progress and discharge procedures, or the production of an inaccurate discharge letter.
- Issues regarding consent were also prevalent in complaints.
- Failures and delays to diagnose were alleged in some of the cases. These include alleged delay in undertaking further tests/procedures, for example colonoscopy and alleged failure to diagnose bowel cancer.
- Improper rectal examinations or sigmoidoscopies, including inadequate consent, inappropriate comments, painful examinations or no chaperone.
- Some complainants reported being unhappy with their doctor’s manner and attitude, and rudeness during the consultation. Some of these communication issues resulted in the patient feeling that the proposed procedure had not been adequately explained to them.
Regulatory (GMC) and disciplinary cases: common themes
Regulatory and disciplinary cases can come from patients and senior or junior colleagues and can be related to clinical and non-clinical issues.
- Performance concerns: operative/clinical skills, clinical judgment and communication.
- Inappropriate personal behaviour/misconduct/boundaries and poor communication with colleagues.
- Probity concerns including incorrect coding and billing.
- Inappropriate delegation or supervision.
- Member health issues including alcohol and drug addictions.
Inquests
Medical Protection has assisted members in writing statements and attending coroners’ inquests. An inquest is a fact-finding exercise that is conducted by the coroner and, in some cases, in front of a jury. The purpose of an inquest is to find out who died – when, where, how and in what circumstances. Medical Protection’s Inquest factsheet gives further information about what happens at an inquest.
Members have requested assistance from Medical Protection with inquests where patients had died following perforations during endoscopic procedures.
- From our analysis, in most of these cases the perforation occurred whilst performing ERCP.
- Perforations occurred in other endoscopic procedures such as colonoscopy and gastroscopy.
- The other cases were regarding death following thromboembolism, liver failure/disease, pancreatic cancer, aspiration pneumonia and myocardial infarction.
Gastroenterology in the UK: Top tips to minimise risk
Please note this is not an exhaustive list of recommendations but key learning points from
our analysis:
- Ensure your endoscopic technique is in line with current best practice such that it
would be supported by your peers. - Keep up to date with current BSG and NICE guidelines. Be aware if new information
becomes available in relation to surveillance intervals or risk of disease. - To reduce the risk of delays in diagnosis explain the uncertainty about the cause of
symptoms to patients, ensuring they understand why, when and with whom they
should re-consult about which concerning symptoms. - Listen to what your patient would consider to be a successful outcome. Understand
your patient’s concerns and expectations. - Discuss the possible benefits and risks of all potential treatment options. Consider
what is most important to that individual, given their specific circumstances. - Explain about frequent and serious complications and the implications for
the individual patient if these occurred. Explain what you would do to correct
complications. - Explain what the procedure will involve, the likely results and when you will see the
patient afterwards. - Double check that the information has been understood and decisions are correctly
informed. Never pressurise or rush patients into giving consent to have an endoscopy. - Clearly document all the steps to provide evidence of a detailed interactive discussion:
this is vital for legal purposes. - Be aware that there are risks associated with delegating giving advice and taking
consent, for example the patient may be dissatisfied and claim later that they did not
fully understand the procedure. - For elective procedures always leave sufficient time (for example at least a week) after
the consultation before scheduling the procedure to allow patients time to think things
through, talk to their family or access more information. - Ensure an endoscopy safer checklist/proforma is completed including:
- patient identity
- proposed procedure indication and consent
- preference for sedation
- relevant comorbidities for example, anticoagulation, drug allergies
- correctly functioning equipment
- correctly labelled histology samples
- clear follow up plan, including informing patients of the results of investigations. - Ensure close monitoring takes place after endoscopy and any deterioration is managed in a timely and appropriate fashion.
- When things go wrong the vast majority of patients just want two things: an
explanation and an apology. - Ensure you are fully indemnified to carry out the relevant procedures in the UK.

From other organisations